How Many Do Babies Bhave What Age Do Bones Stop Growing
Learning Outcomes
- Describe how bones develop, abound, and repair
Ossification, or osteogenesis, is the process of bone germination by osteoblasts. Ossification is distinct from the process of calcification; whereas calcification takes place during the ossification of bones, it can also occur in other tissues. Ossification begins approximately six weeks after fertilization in an embryo. Before this time, the embryonic skeleton consists entirely of fibrous membranes and hyaline cartilage. The evolution of bone from fibrous membranes is called intramembranous ossification; development from hyaline cartilage is chosen endochondral ossification. Bone growth continues until approximately age 25. Bones can grow in thickness throughout life, but after age 25, ossification functions primarily in bone remodeling and repair.
Intramembranous Ossification
Intramembranous ossification is the process of bone evolution from gristly membranes. Information technology is involved in the germination of the apartment bones of the skull, the mandible, and the clavicles. Ossification begins as mesenchymal cells course a template of the hereafter bone. They so differentiate into osteoblasts at the ossification center. Osteoblasts secrete the extracellular matrix and deposit calcium, which hardens the matrix. The not-mineralized portion of the bone or osteoid continues to grade around claret vessels, forming spongy bone. Connective tissue in the matrix differentiates into cherry-red bone marrow in the fetus. The spongy bone is remodeled into a sparse layer of compact bone on the surface of the spongy bone.
Endochondral Ossification
Endochondral ossification is the process of bone development from hyaline cartilage. All of the bones of the body, except for the flat bones of the skull, mandible, and clavicles, are formed through endochondral ossification.
In long bones, chondrocytes form a template of the hyaline cartilage diaphysis. Responding to complex developmental signals, the matrix begins to calcify. This calcification prevents improvidence of nutrients into the matrix, resulting in chondrocytes dying and the opening upwardly of cavities in the diaphysis cartilage. Blood vessels invade the cavities, and osteoblasts and osteoclasts modify the calcified cartilage matrix into spongy bone. Osteoclasts then intermission down some of the spongy bone to create a marrow, or medullary, cavity in the centre of the diaphysis. Dumbo, irregular connective tissue forms a sheath (periosteum) effectually the bones. The periosteum assists in attaching the bone to surrounding tissues, tendons, and ligaments. The os continues to grow and elongate as the cartilage cells at the epiphyses divide.
In the last stage of prenatal os evolution, the centers of the epiphyses begin to calcify. Secondary ossification centers form in the epiphyses equally blood vessels and osteoblasts enter these areas and convert hyaline cartilage into spongy bone. Until adolescence, hyaline cartilage persists at the epiphyseal plate (growth plate), which is the region between the diaphysis and epiphysis that is responsible for the lengthwise growth of long bones (Figure i).
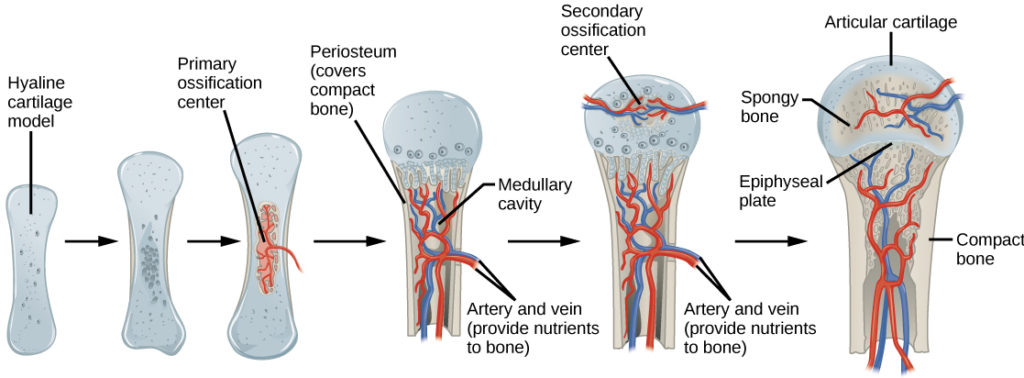
Figure i. Endochondral ossification is the process of bone development from hyaline cartilage. The periosteum is the connective tissue on the exterior of bone that acts equally the interface betwixt os, blood vessels, tendons, and ligaments.
Growth of Bone
Long basic continue to lengthen, potentially until adolescence, through the add-on of bone tissue at the epiphyseal plate. They besides increase in width through appositional growth.
Lengthening of Long Basic
Chondrocytes on the epiphyseal side of the epiphyseal plate divide; one prison cell remains undifferentiated almost the epiphysis, and i jail cell moves toward the diaphysis. The cells, which are pushed from the epiphysis, mature and are destroyed by calcification. This procedure replaces cartilage with bone on the diaphyseal side of the plate, resulting in a lengthening of the bone.
Long basic cease growing at effectually the age of xviii in females and the age of 21 in males in a process called epiphyseal plate closure. During this process, cartilage cells stop dividing and all of the cartilage is replaced by bone. The epiphyseal plate fades, leaving a construction chosen the epiphyseal line or epiphyseal remnant, and the epiphysis and diaphysis fuse.
Thickening of Long Basic
Appositional growth is the increase in the diameter of bones by the addition of bony tissue at the surface of bones. Osteoblasts at the bone surface secrete bone matrix, and osteoclasts on the inner surface break downwards bone. The osteoblasts differentiate into osteocytes. A residuum between these two processes allows the os to thicken without becoming likewise heavy.
Bone Remodeling and Repair
Bone renewal continues later on birth into adulthood. Bone remodeling is the replacement of old bone tissue by new os tissue. Information technology involves the processes of bone degradation by osteoblasts and os resorption by osteoclasts. Normal bone growth requires vitamins D, C, and A, plus minerals such as calcium, phosphorous, and magnesium. Hormones such as parathyroid hormone, growth hormone, and calcitonin are also required for proper bone growth and maintenance.
Os turnover rates are quite high, with five to seven pct of os mass being recycled every week. Differences in turnover charge per unit exist in different areas of the skeleton and in dissimilar areas of a bone. For example, the os in the caput of the femur may be fully replaced every six months, whereas the bone along the shaft is altered much more slowly.

Figure 2. Afterwards this os is set, a callus will knit the two ends together. (credit: Bill Rhodes)
Os remodeling allows bones to suit to stresses by becoming thicker and stronger when subjected to stress. Basic that are not discipline to normal stress, for instance when a limb is in a cast, will brainstorm to lose mass. A fractured or broken bone undergoes repair through 4 stages:
- Blood vessels in the broken bone tear and hemorrhage, resulting in the formation of clotted blood, or a hematoma, at the site of the break. The severed blood vessels at the cleaved ends of the bone are sealed by the clotting procedure, and bone cells that are deprived of nutrients brainstorm to dice.
- Within days of the fracture, capillaries abound into the hematoma, and phagocytic cells brainstorm to clear away the dead cells. Though fragments of the blood jell may remain, fibroblasts and osteoblasts enter the area and begin to reform os. Fibroblasts produce collagen fibers that connect the broken bone ends, and osteoblasts start to grade spongy bone. The repair tissue between the broken os ends is called the fibrocartilaginous callus, as information technology is composed of both hyaline and fibrocartilage (Figure 2). Some bone spicules may also appear at this point.
- The fibrocartilaginous callus is converted into a bony callus of spongy bone. It takes about two months for the broken os ends to exist firmly joined together after the fracture. This is similar to the endochondral formation of bone, as cartilage becomes ossified; osteoblasts, osteoclasts, and bone matrix are present.
- The bony callus is then remodelled by osteoclasts and osteoblasts, with excess textile on the exterior of the os and within the medullary cavity beingness removed. Compact bone is added to create bone tissue that is similar to the original, unbroken bone. This remodeling can accept many months, and the bone may remain uneven for years.
Decalcification of Bones
Question: What upshot does the removal of calcium and collagen take on bone construction?
Background: Deport a literature search on the role of calcium and collagen in maintaining bone structure. Conduct a literature search on diseases in which bone structure is compromised.
Hypothesis: Develop a hypothesis that states predictions of the flexibility, strength, and mass of basic that have had the calcium and collagen components removed. Develop a hypothesis regarding the attempt to add calcium back to decalcified bones.
Exam the hypothesis: Examination the prediction by removing calcium from chicken bones past placing them in a jar of vinegar for seven days. Test the hypothesis regarding adding calcium back to decalcified bone by placing the decalcified chicken bones into a jar of water with calcium supplements added. Test the prediction by denaturing the collagen from the bones by baking them at 250°C for three hours.
Analyze the data: Create a table showing the changes in bone flexibility, strength, and mass in the three different environments.
Report the results: Under which weather condition was the bone virtually flexible? Nether which weather was the bone the strongest?
Draw a determination: Did the results support or abnegate the hypothesis? How practise the results observed in this experiment stand for to diseases that destroy os tissue?
IN SUMMARY: Bone Growth and Evolution
Ossification is the procedure of bone formation by osteoblasts. Intramembranous ossification is the process of bone development from gristly membranes. Endochondral ossification is the procedure of bone development from hyaline cartilage. Long bones lengthen every bit chondrocytes dissever and secrete hyaline cartilage. Osteoblasts replace cartilage with os. Appositional growth is the increase in the diameter of bones past the addition of bone tissue at the surface of bones. Bone remodeling involves the processes of bone deposition by osteoblasts and bone resorption past osteoclasts. Os repair occurs in iv stages and can take several months.
Try It
Contribute!
Did you have an idea for improving this content? We'd love your input.
Improve this pageLearn More than
Source: https://courses.lumenlearning.com/wm-biology2/chapter/bone-growth-and-development/
0 Response to "How Many Do Babies Bhave What Age Do Bones Stop Growing"
Post a Comment